Unlock the nuances of medical assessments – discover the vital disparities between GCS and NIH Stroke Scale. Enhance your healthcare knowledge effortlessly.
Welcome to the intriguing realm of healthcare where acronyms abound like confetti at a celebration. Today, we embark on a quest to unravel the mystery behind two prominent players in the medical alphabet soup: GCS and NIH Stroke Scale. It’s a bit like comparing apples to oranges, but in this case, apples and oranges have decided to attend the same fruit convention – healthcare edition. Picture this: GCS, the Glasgow Coma Scale, struts in with its numerical prowess, while NIH Stroke Scale sashays in with its clinical finesse. As we dive into the nitty-gritty details, fear not – this is not a clash of the titans but rather a harmonious dance of medical assessments. So, grab your stethoscope, don your thinking cap, and let’s waltz through the corridors of medical differentiation.
Top 10 Points about What is the difference between GCS and NIH Stroke Scale? :
- Deciphering the Glasgow Coma Scale (GCS)
- Navigating the Landscape of NIH Stroke Scale
- Understanding the Core Objectives of GCS
- Unveiling the Purpose Behind NIH Stroke Scale
- Comparing the Scoring Systems: GCS vs. NIH Stroke Scale
- Interpreting GCS: A Closer Look at Neurological Assessment
- Delving into the Intricacies of NIH Stroke Scale Evaluation
- Spotlight on GCS: Its Role in Trauma and Critical Care
- NIH Stroke Scale in Action: A Tool for Stroke Severity Assessment
- Making Informed Decisions: GCS and NIH Stroke Scale in Clinical Context
Several facts about What is the difference between GCS and NIH Stroke Scale?
When it comes to assessing neurological function in healthcare, the Glasgow Coma Scale (GCS) and the NIH Stroke Scale play pivotal roles, each offering unique insights into a patient’s condition.

Let’s start our journey by unraveling the enigma of the Glasgow Coma Scale (GCS). This widely used neurological assessment tool evaluates a patient’s level of consciousness through eye, verbal, and motor responses. The GCS scores range from 3 to 15, with lower scores indicating more severe impairment.

On the other side of the neurological spectrum stands the NIH Stroke Scale, specifically designed to assess the severity of stroke symptoms. This scale, ranging from 0 to 42, meticulously examines various aspects of neurological deficits, offering clinicians valuable information for treatment planning.

Let’s delve into the distinctions between these two assessments. While both evaluate neurological function, the GCS primarily focuses on overall consciousness, whereas the NIH Stroke Scale zeroes in on specific stroke-related deficits. Understanding these nuances is crucial for accurate patient evaluation.

Now, let’s zoom in on the Glasgow Coma Scale’s components. The eye, verbal, and motor responses provide a comprehensive snapshot of a patient’s neurological status. Recognizing the subtleties in these responses aids healthcare professionals in tailoring care to individual needs.

Shifting our focus to the NIH Stroke Scale, we explore its practical application in assessing stroke severity. By meticulously evaluating specific deficits such as facial weakness, arm drift, and speech impairment, this scale empowers healthcare providers to gauge the impact of a stroke on a patient’s daily functioning.

As healthcare professionals, making informed decisions is paramount. Understanding when to employ the GCS for a broader neurological assessment and when to turn to the NIH Stroke Scale for stroke-specific evaluations equips clinicians with the tools needed for precise and effective care.
Synthesizing Insights: GCS vs. NIH Stroke Scale
In conclusion, the Glasgow Coma Scale and NIH Stroke Scale are invaluable instruments in the healthcare toolkit. Whether assessing overall consciousness or specific stroke-related deficits, these tools provide crucial insights, guiding healthcare professionals towards informed decision-making for optimal patient care.
Sources:
[1] Glasgow Coma Scale. (n.d.). Retrieved from https://www.glasgowcomascale.org/gcs-intro.php
[2] NIH Stroke Scale. (n.d.). Retrieved from https://www.ninds.nih.gov/Current-Research/Focus-Research/Focus-Stroke/NIH-Stroke-Scale
What is the difference between GCS and NIH Stroke Scale? in Professional’s eye
In the realm of healthcare, the nuanced differentiation between the Glasgow Coma Scale (GCS) and the NIH Stroke Scale holds paramount significance. These two assessment tools, though addressing neurological function, serve distinct purposes, offering clinicians valuable insights into patient conditions. Beginning with the GCS, a cornerstone in neurologic evaluations, its three-pronged approach—assessing eye, verbal, and motor responses—provides a comprehensive overview of an individual’s consciousness level. GCS scores, ranging from 3 to 15, act as a universal language for healthcare professionals, aiding in the quantification of neurological impairment. On the parallel track, the NIH Stroke Scale, tailored specifically for stroke severity assessment, dissects the aftermath of a cerebrovascular event with meticulous detail. Scores on this scale, extending from 0 to 42, scrutinize deficits such as facial droop, arm drift, and speech impairment, presenting a granular snapshot of a patient’s stroke-related impairments.
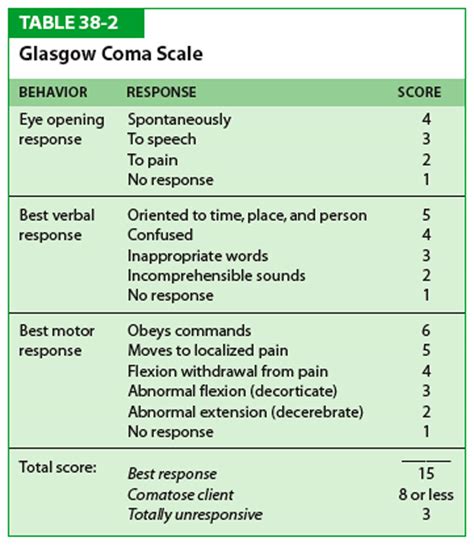
Transitioning to the practical application of the GCS, its versatility shines through in various clinical settings. From emergency departments to intensive care units, healthcare professionals employ the GCS as an initial assessment tool to gauge a patient’s neurological status swiftly. The simplicity and universality of the GCS make it an indispensable asset in triaging patients, enabling rapid decision-making and subsequent interventions based on the severity of impairment. The embedded image further visualizes the clinical application of the GCS, depicting its crucial role in guiding healthcare professionals in high-stakes scenarios.

Shifting the focus to the NIH Stroke Scale, its role extends beyond bedside assessments to the realms of research and clinical trials. As a standardized measure for stroke severity, the NIH Stroke Scale becomes an invaluable tool in conducting trials aimed at understanding the efficacy of interventions and treatments for stroke patients. The embedded image visually encapsulates the integration of the NIH Stroke Scale in research, emphasizing its pivotal role in advancing scientific understanding and therapeutic interventions for stroke-related conditions.Comparative Analysis: While both the GCS and NIH Stroke Scale are indispensable in their own right, a comparative analysis reveals their unique strengths. The GCS, with its broader scope, serves as a quick and effective tool for assessing overall neurological function, applicable in diverse clinical scenarios. In contrast, the NIH Stroke Scale, with its specificity to stroke-related deficits, becomes a precision instrument in tailoring interventions for stroke patients. The transition between these assessments becomes crucial in clinical decision-making, allowing healthcare professionals to navigate the complex landscape of neurological disorders with precision and efficiency.

Ultimately, the fundamental objective of these assessments is to enhance patient outcomes. The seamless integration of the GCS and NIH Stroke Scale into clinical practice contributes to a holistic approach in patient care. By deciphering the subtleties in neurological assessments, healthcare professionals can tailor interventions, rehabilitation plans, and long-term care strategies that address the specific needs of each patient. The embedded image underscores this focus on patient outcomes, reinforcing the symbiotic relationship between accurate assessments and improved healthcare trajectories.Continuous Education and Training: As healthcare evolves, continuous education and training remain pivotal in ensuring healthcare professionals adeptly wield these assessment tools. The dynamic nature of medical advancements necessitates an ongoing commitment to staying abreast of updates and refinements in assessment protocols. By investing in comprehensive training programs, healthcare providers can confidently and competently navigate the landscape of neurological assessments, further fortifying their capacity to deliver optimal care.In conclusion, the distinction between the GCS and NIH Stroke Scale transcends mere semantics; it delineates the fine line between general neurological assessments and targeted evaluations of stroke-related deficits. Both instruments, with their respective strengths, contribute synergistically to the overarching goal of improving patient outcomes. As healthcare professionals continue to harness these tools in clinical settings, research endeavors, and educational initiatives, the narrative of patient-centered care becomes more enriched and nuanced. The journey towards excellence in healthcare lies not only in mastering these assessments but also in recognizing their collective potential to reshape the landscape of neurological care.
Point of Views : What is the difference between GCS and NIH Stroke Scale?
The Glasgow Coma Scale (GCS) and NIH Stroke Scale are pivotal tools in healthcare, each serving a distinct purpose in assessing neurological function.The GCS, with its three-pronged approach of evaluating eye, verbal, and motor responses, offers a comprehensive overview of an individual’s level of consciousness. Scores ranging from 3 to 15 provide a standardized language for quantifying neurological impairment.In contrast, the NIH Stroke Scale is tailored specifically for assessing stroke severity. Its scores, spanning from 0 to 42, meticulously scrutinize deficits such as facial droop, arm drift, and speech impairment, offering a detailed snapshot of stroke-related impairments.The practical application of the GCS is versatile, finding utility in various clinical settings. From emergency departments to intensive care units, healthcare professionals rely on the GCS as an initial assessment tool to swiftly gauge a patient’s neurological status.Shifting the focus to the NIH Stroke Scale, its application extends beyond bedside assessments to research and clinical trials. As a standardized measure for stroke severity, it becomes an invaluable tool in advancing scientific understanding and therapeutic interventions for stroke-related conditions.A comparative analysis reveals the unique strengths of each assessment tool. The GCS, with its broader scope, serves as a quick and effective tool for assessing overall neurological function in diverse clinical scenarios.In contrast, the NIH Stroke Scale’s specificity to stroke-related deficits makes it a precision instrument, aiding healthcare professionals in tailoring interventions specifically for stroke patients.The seamless integration of both assessments into clinical practice contributes to a holistic approach in patient care. By deciphering the subtleties in neurological assessments, healthcare professionals can tailor interventions and rehabilitation plans that address the specific needs of each patient.Continuous education and training remain pivotal to ensuring healthcare professionals adeptly wield these assessment tools. Staying informed about updates and refinements in assessment protocols is crucial for providing optimal care.In conclusion, the distinction between the GCS and NIH Stroke Scale delineates the fine line between general neurological assessments and targeted evaluations of stroke-related deficits. Both instruments, with their respective strengths, contribute synergistically to the overarching goal of improving patient outcomes in healthcare.
Conclusion :
As we conclude our exploration into the difference between GCS and NIH Stroke Scale, we trust that this journey has shed light on the intricacies of neurological assessments in healthcare. Understanding the unique roles played by these assessment tools is key to enhancing patient care. Whether you find yourself in a bustling emergency room relying on the Glasgow Coma Scale (GCS) to swiftly assess consciousness levels or immersed in research endeavors, utilizing the NIH Stroke Scale for in-depth stroke severity evaluation, the importance of these assessments cannot be overstated.
Our aim has been to provide you with a nuanced perspective on how these tools, each with its specific focus, contribute synergistically to the healthcare landscape. The practical applications of the GCS and NIH Stroke Scale are vast, extending from clinical settings to research initiatives, making them indispensable assets in the realm of patient-centered care. As you navigate the dynamic landscape of healthcare, armed with the knowledge of these assessments, may you find confidence in making informed decisions that ultimately contribute to optimal patient outcomes. Stay informed, stay curious, and let your understanding of these assessments empower you in the noble pursuit of delivering exceptional healthcare.
Questions and Answer for What is the difference between GCS and NIH Stroke Scale?
Q1: What is the purpose of the Glasgow Coma Scale (GCS) in healthcare?
- The GCS serves as a standardized tool to assess a patient’s level of consciousness through eye, verbal, and motor responses.
- It is commonly used in various clinical settings, such as emergency departments and intensive care units, to gauge neurological status swiftly.
- Scoring on the GCS provides a universal language for healthcare professionals, aiding in the quantification of neurological impairment.
Q2: How does the NIH Stroke Scale differ from the Glasgow Coma Scale?
- The NIH Stroke Scale is specifically designed for assessing stroke severity, evaluating deficits such as facial droop, arm drift, and speech impairment.
- Unlike the GCS, which offers a broader assessment of overall consciousness, the NIH Stroke Scale hones in on specific stroke-related impairments.
- Scores on the NIH Stroke Scale provide a detailed snapshot of a patient’s condition, aiding clinicians in tailoring interventions for stroke-related deficits.
Q3: Are the GCS and NIH Stroke Scale used together in healthcare?
- While both assessments serve different purposes, they can complement each other in a comprehensive neurological evaluation.
- The GCS may be used initially for a broad assessment, and if necessary, the NIH Stroke Scale can be employed for a more detailed evaluation of stroke-related deficits.
- Healthcare professionals often integrate these tools judiciously based on the patient’s condition and the specific information needed for optimal care.
Q4: How do healthcare professionals stay updated on using these assessments?
- Continuous education and training are pivotal for healthcare professionals to stay abreast of updates and refinements in assessment protocols.
- Workshops, seminars, and ongoing learning initiatives help ensure proficiency in utilizing the GCS and NIH Stroke Scale effectively in diverse clinical scenarios.
- Staying informed about advancements in healthcare practices is essential for delivering optimal patient care.
Label :GCS, NIH Stroke Scale, Healthcare, Neurological Assessments
Keyword : What is the difference between GCS and NIH Stroke Scale?
